The clinical definition of empathy in a healthcare context is the ability to understand a patient’s situation, perspective, and feelings, to communicate that understanding back to the patient, and to act upon that understanding in a therapeutic way. It is a multi-layered cognitive and emotional skill, distinct from sympathy, which involves feeling for someone, often accompanied by pity. Empathy is about feeling with someone, a shared human experience that bridges the gap between caregiver and patient. This distinction is crucial; sympathy can create distance, while empathy fosters connection and partnership in the healing process.
The physiological impact of empathic care is profound and measurable. When a healthcare provider engages with genuine empathy, it activates the patient’s parasympathetic nervous system, reducing the production of stress hormones like cortisol. This biochemical shift lowers heart rate and blood pressure, creating an internal environment more conducive to healing. Studies have shown that patients who perceive their doctors as empathetic experience better control of their hemoglobin A1c levels in diabetes and higher rates of adherence to medication regimens. The simple act of feeling heard and understood can modulate the immune response, reduce the perception of pain, and decrease the length of hospital stays. Empathy is not a soft, fluffy add-on; it is a tangible, evidence-based clinical tool that directly influences patient outcomes.
Effective communication is the primary vehicle for delivering empathy. It begins with active listening, which involves giving a patient one’s full attention, free from the distraction of a computer screen or a chart. It means listening to understand, not simply to respond or diagnose. Techniques like reflective statements (“It sounds like you’ve been feeling very overwhelmed by this new diagnosis”) and validating emotions (“That is completely understandable, anyone in your situation would feel scared”) confirm the patient’s experience. Open-ended questions (“What’s been on your mind since your last visit?”) invite patients to share more than just a list of symptoms, revealing crucial contextual information about their lives, fears, and goals. This dialogue builds a shared understanding from which a truly collaborative treatment plan can emerge.
The diagnostic process itself is deeply enhanced by an empathic approach. A patient’s story, or narrative, contains vital clues that pure biometric data can miss. A rushed clinician may overlook the significance of a patient mentioning financial stress, loneliness, or caregiving responsibilities—all social determinants of health that directly impact physical well-being. An empathetic provider, by creating a safe space for the patient to unveil these details, gains a holistic view of the illness. This context transforms a generic treatment protocol into a personalized plan that the patient is more likely to follow. For instance, understanding that a patient cannot afford a specific medication or lacks transportation to physical therapy appointments allows the provider to problem-solve with the patient, connecting them with social workers or community resources, thereby making the prescribed care actually feasible.
For the patient, the experience of empathic care is transformative. It replaces feelings of fear, vulnerability, and anonymity with those of safety, dignity, and partnership. A diagnosis, particularly a serious one, can be an isolating experience. An empathetic clinician mitigates this isolation, making the patient feel they are not facing their illness alone. This psychological safety reduces anxiety and empowers the patient to engage actively in their own care. It builds trust, which is the absolute foundation of the therapeutic relationship. When patients trust their providers, they are more honest about their symptoms, their struggles with treatment, and their lifestyle choices, leading to more accurate care and better health outcomes. This human connection is often what patients remember long after the clinical details fade.
The demands on healthcare professionals are immense, leading to high rates of burnout characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. Ironically, while often seen as a drain, the practice of empathy can be a powerful buffer against this burnout. Connecting with patients on a human level reinforces the meaning and purpose behind the demanding work. It shifts the dynamic from transactional, task-oriented interactions to meaningful relationships that are inherently more fulfilling. Healthcare systems that prioritize and train for empathy see higher staff satisfaction and lower turnover rates. Protecting time for appointments, providing communication training, and fostering a culture that values the patient-provider relationship are essential investments in sustaining the workforce.
The integration of technology, particularly the widespread adoption of Electronic Health Records (EHRs), presents a significant challenge to empathetic interaction. The screen in the examination room can become a literal barrier, pulling the clinician’s focus away from the person and toward data entry. This “distracted doctoring” leads to patients feeling unheard and dissatisfied. Overcoming this requires intentional effort. Techniques such as positioning the computer to maintain eye contact, typing only after the patient has finished speaking, and using narrative notes to capture the patient’s story rather than just bullet-pointed facts can help. The goal is to use technology as a tool to enhance, rather than replace, the human connection. Telehealth further complicates this dynamic, requiring providers to be even more deliberate in their verbal cues and active listening skills to convey empathy without physical presence.
Systemic and institutional barriers within modern healthcare often actively work against empathy. Productivity pressures that mandate short appointment times, overwhelming administrative burdens, and financial models that prioritize volume over value create an environment where empathy is treated as a luxury rather than a necessity. Cultivating a truly empathetic culture requires a top-down commitment. This includes redesigning workflows to protect patient-clinician time, incorporating patient satisfaction scores related to communication into performance metrics, and providing robust training programs. These programs should move beyond simple communication技巧 to include narrative medicine, which uses literature and patient stories to build empathy, and role-playing exercises to practice difficult conversations. Institutions must recognize that empathy is a core clinical skill that requires the same level of attention and resource allocation as technical proficiency.
The measurement of empathy in healthcare settings, while challenging, is critical for improvement. Patient-reported experience measures (PREMs) and specific survey tools provide direct feedback on how patients perceive their care. These can include questions about whether the doctor listened carefully, explained things clearly, showed respect, and spent enough time with them. For clinicians, tools like the Jefferson Scale of Empathy offer a self-assessment of their empathetic orientation. Combining this data creates a feedback loop for both individual providers and the entire system, identifying areas for growth and highlighting successes. This data-driven approach allows healthcare organizations to move from abstract values to concrete, improvable actions, ensuring that the human touch remains a measurable and prioritized component of high-quality care.
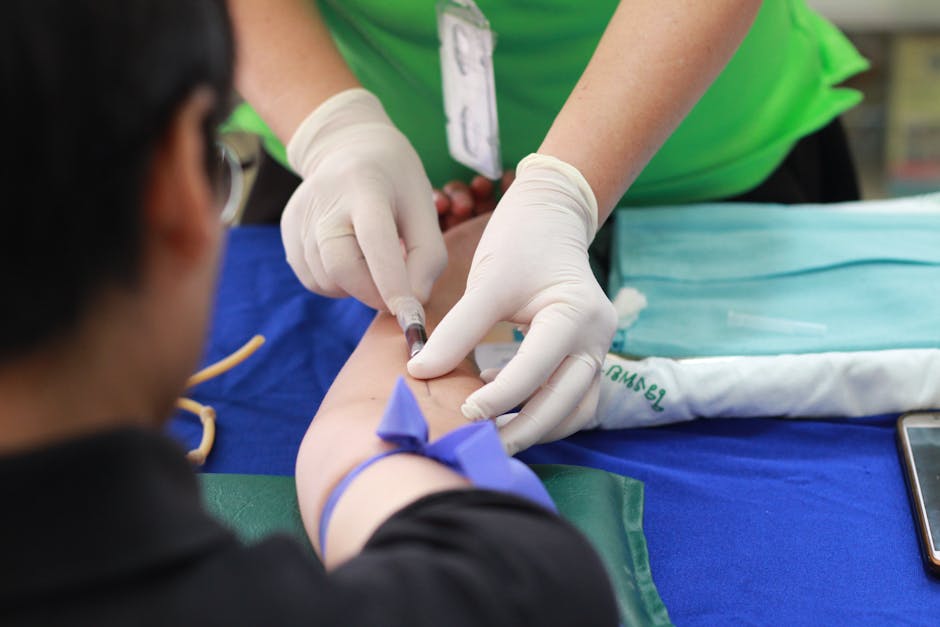
Empathy must extend beyond the individual clinician-patient dyad to encompass the entire design of the healthcare experience. This includes the compassion shown by a receptionist scheduling an appointment, the kindness of a phlebotomist during a blood draw, and the clear communication from a billing specialist. Environmental design plays a role: calming waiting areas, clear signage, and private spaces for difficult conversations all contribute to an empathetic ecosystem. It involves creating patient portals that are easy to navigate and providing translation services for non-native speakers. A truly empathetic system anticipates patient anxiety and confusion at every touchpoint and works to alleviate it through thoughtful, human-centered design. This holistic approach ensures that empathy is not a sporadic event but a consistent, reliable characteristic of the entire care journey.
The legal and ethical dimensions of healthcare are also deeply intertwined with empathy. Informed consent, for example, is not merely a signature on a form but a process of ensuring a patient truly understands the risks, benefits, and alternatives to a procedure. This process requires empathy to gauge the patient’s level of comprehension, address their specific fears, and ensure their agreement is voluntary and informed. In navigating medical errors or adverse outcomes, an empathetic approach is the cornerstone of ethical disclosure and apology, which is not only the right thing to do but also mitigates legal risk. Furthermore, empathy is fundamental to providing culturally competent care, enabling providers to understand and respect the health beliefs, practices, and linguistic needs of diverse patient populations, thereby addressing disparities and promoting health equity.
Ultimately, the human touch in healthcare, embodied by empathy, is what transforms a clinical encounter into a healing relationship. It is the critical element that allows science and technology to be applied effectively to the complex reality of a human life. In an era of advancing technology and increasing systemic pressures, protecting and prioritizing this human connection is not a nostalgic wish but a strategic imperative for achieving the triple aim of better care, improved population health, and lower per capita costs. The practice of empathy requires continuous effort, deliberate practice, and systemic support, but its回报 is immeasurable: care that is not only technically excellent but also profoundly compassionate, recognizing and honoring the humanity of both the patient and the provider in the shared pursuit of health.